UK GPs Grapple with Rising Multimorbidity as Patient Care Evolves
Research reveals UK GPs spend over a third of their time on patients with multiple chronic conditions. Appointment durations increase while frequency decreases, reflecting changing healthcare dynamics.

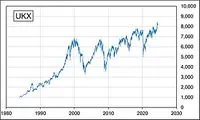
Recent research has unveiled a significant shift in the workload of General Practitioners (GPs) in the United Kingdom. The study, published in the British Journal of General Practice, analyzed data from over 10 million patients across 824 GP surgeries between 2005 and 2019.
The findings indicate that GPs are dedicating an increasing amount of time to patients with multiple chronic conditions. Despite representing only 16% of the population, individuals with three or more serious chronic illnesses now account for 34.5% of a GP's patient time annually. This marks a substantial increase from 22.5% in 2005.

The rise in multimorbidity is evident, with the proportion of people having three or more long-term illnesses nearly doubling from 9.7% in 2005 to 16% in 2019. This translates to approximately 10.6 million individuals across the country. Concurrently, the percentage of patients without serious chronic conditions has decreased from 51.5% to 43.6%.
Interestingly, while GPs are spending more time with patients with complex health needs, the overall frequency of appointments has declined. The average number of GP consultations per patient fell from 3.84 in 2014 to 3.47 in 2019. However, the duration of these appointments has increased by 36% since 2005, from just over six minutes to almost nine minutes in 2019.
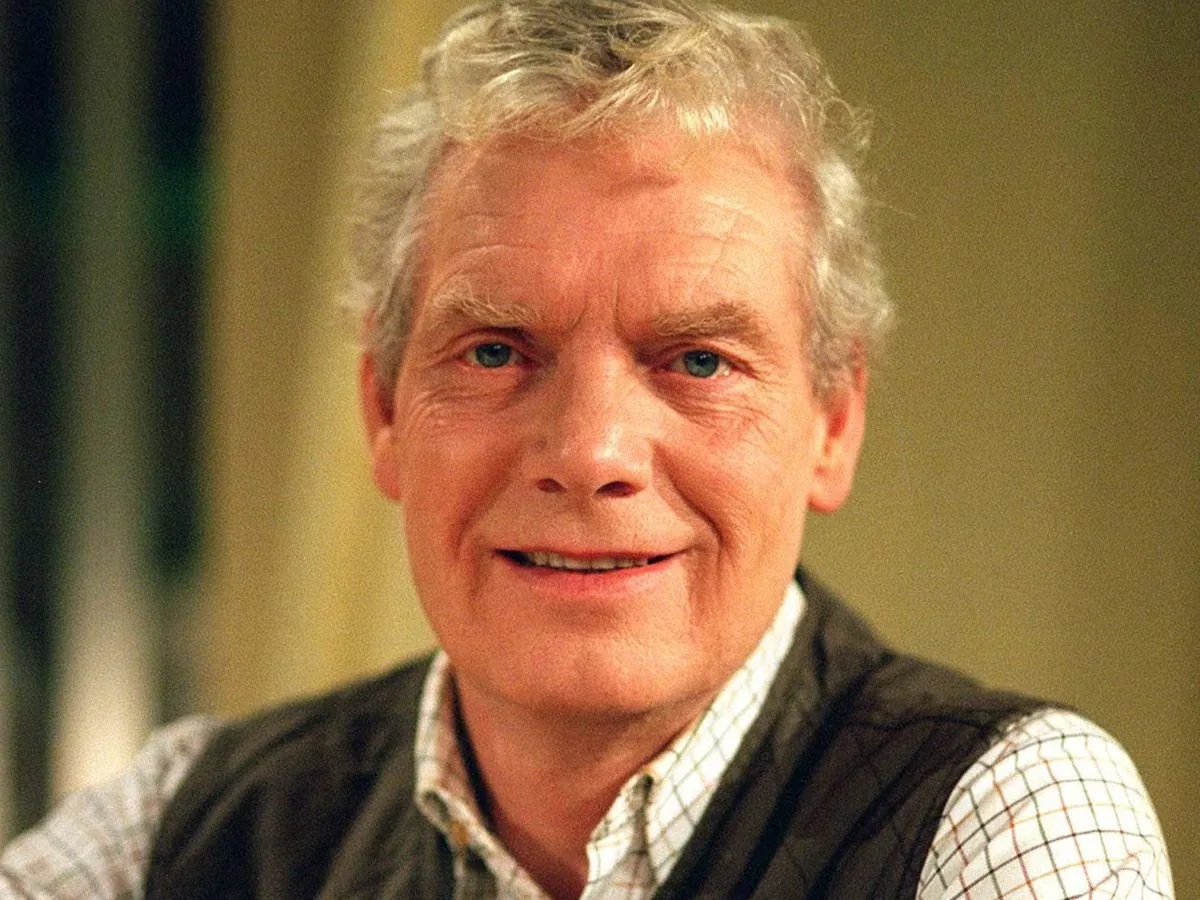
Prof Kamila Hawthorne, chairman of the Royal College of General Practitioners, highlighted the challenges faced by GPs in caring for an aging population with complex health issues. She noted that the increasing administrative responsibilities, which now consume about a quarter of a GP's total time, are diverting attention from direct patient care.
The study's findings align with global health trends. The World Health Organization estimates that chronic diseases are responsible for 71% of all deaths globally, underscoring the growing importance of managing multiple long-term conditions.
In response to these challenges, Wes Streeting, the Health Secretary, has called for improved patient access to GP services. He stated, "The front door to the NHS is broken. GPs are overstretched and far too many patients are finding it impossible to get an appointment when they need one."
"The front door to the NHS is broken. GPs are overstretched and far too many patients are finding it impossible to get an appointment when they need one."
The situation has led to various forms of protest action by GPs in England, including capping daily appointment numbers. In response, the government recently awarded an above-inflation boost of 7.4% to their "global sum" funding, amounting to about £500 million.
As the NHS faces these challenges, a parallel trend is emerging among younger generations. A survey commissioned by the Independent Healthcare Providers Network found that 44% of people in their 20s and 30s would consider private healthcare if needed in the next 12 months. This shift reflects changing attitudes towards healthcare provision and may signal future trends in the UK's healthcare landscape.
The evolving nature of patient care, coupled with the increasing prevalence of multimorbidity, presents both challenges and opportunities for the UK's healthcare system. As GPs adapt to these changes, the focus remains on providing effective care for an aging population with increasingly complex health needs.