Staffing Crisis at Chester Hospital Preceded Letby's Crimes
Years of budget cuts and staff shortages at Countess of Chester Hospital's neonatal unit created a "perfect storm" before Lucy Letby's crimes. An inquiry is set to investigate the issues.
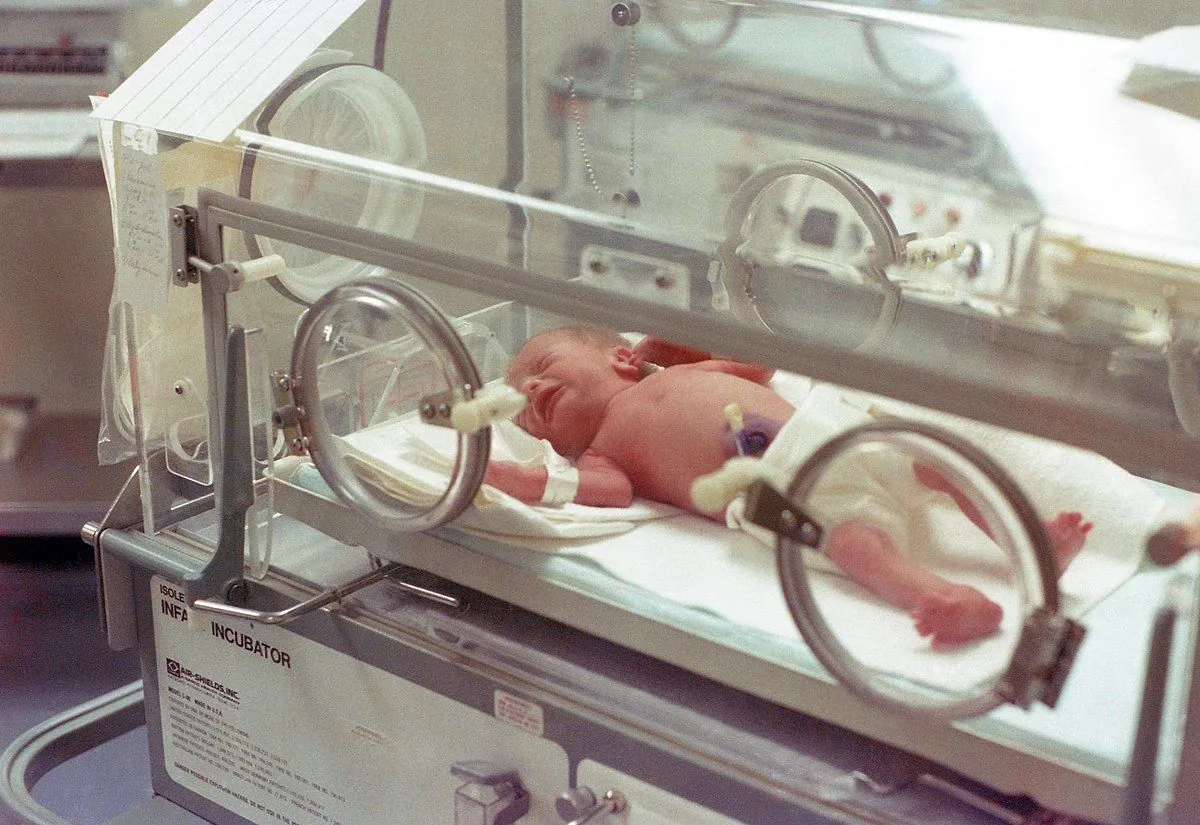
The neonatal unit at Countess of Chester Hospital, where Lucy Letby worked, faced severe staffing issues and budget cuts for years before her crimes came to light. This situation has been described as an "accident waiting to happen" by former staff members.
In August 2023, Letby was convicted of murdering seven babies and attempting to murder six others at the hospital's neonatal unit in 2015 and 2016. A retrial in 2024 found her guilty of attempting to murder another child, known as Baby K.
However, the roots of the problem stretch back much further. In 2004, twenty years before the inquiry set to begin in September 2024, nurses at the unit wrote a letter expressing "grave concerns" about staffing levels. They warned of an "increased risk of clinical incidents" due to the "continual excessive workload."
"The hospital said they would no longer need ANNPs because they would not be caring for really sick babies. At the time I told management that was ludicrous but it fell on deaf ears."
Despite these warnings, further cuts were made in subsequent years. The unit lost two Advanced Neonatal Nurse Practitioners (ANNPs), specialized nurses introduced in the UK in the 1990s to take on some roles of junior doctors. Michele Worden, an ANNP with 28 years of NHS experience, was made redundant in 2007.
By 2011, eight registered nurses had left the unit, replaced by eight unregulated nursery nurses. The following year, the hospital employed two nurses straight out of university, one of whom was Letby.

The situation continued to deteriorate. Around 2013-2014, junior trainee paediatricians from the School of Medicine at Liverpool University were pulled from the unit, further depleting medical staff. By December 2015, Dr Alison Timmis, a paediatrician, reported to the hospital's chief executive that staff were in tears due to being overworked and lacking vital equipment.
An investigation by the Royal College of Paediatrics and Child Health (RCPCH), established in 1996, found organizational and environmental issues with the ward between 2015 and 2016. The review team uncovered a pattern of "insufficient senior cover and a reluctance to seek advice" from consultants.
These findings highlight a broader context of challenges within the NHS. The establishment of the Care Quality Commission in 2009 and the publication of the Francis Report in 2013, which revealed serious failings in patient care at another NHS trust, underscore the ongoing struggles within the healthcare system.
As the inquiry led by Lady Justice Thirlwall prepares to begin, it will undoubtedly examine how these systemic issues may have contributed to the tragic events at the Countess of Chester Hospital. The investigation will likely consider the impact of budget constraints, staffing shortages, and organizational failures in the context of the NHS's broader challenges, including the unprecedented strain caused by the COVID-19 pandemic beginning in 2020.