Rural England Faces "Pharmacy Deserts" as Closures Mount
Rural areas in England are experiencing a significant decline in pharmacy access, with hundreds of closures since the pandemic. Industry leaders warn of emerging "pharmacy deserts" in isolated regions.

The landscape of healthcare accessibility in rural England is undergoing a concerning transformation, as the number of community pharmacies continues to dwindle. Industry experts are sounding the alarm about the emergence of "pharmacy deserts" in these areas, highlighting a growing disparity in access to essential medical services.
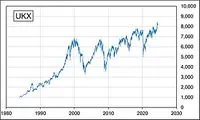
According to an analysis conducted by the National Pharmacy Association (NPA), hundreds of pharmacies have ceased operations since the onset of the COVID-19 pandemic, with rural regions bearing the brunt of these closures. The study reveals a stark reality: 17 out of 20 local council areas with the lowest pharmacy-to-population ratios are situated in rural settings.
This trend is particularly alarming given the vital role pharmacies play in community health. In 2022, approximately 1.1 million people in England sought health advice from pharmacies daily, underscoring their importance as accessible healthcare providers. The average community pharmacy serves around 5,000 patients, making their presence crucial for maintaining public health.

The closure of major pharmacy chains, such as Boots and Lloyds Pharmacy, has exacerbated the situation. As more consumers turn to online services, brick-and-mortar pharmacies in rural towns and villages are shuttering, forcing residents to travel greater distances for their medication needs. This shift is particularly challenging for elderly and less mobile populations who rely heavily on local pharmacy services.
West Berkshire exemplifies the severity of the issue, with a mere 9.9 pharmacies per 100,000 residents—a figure four times lower than Westminster, which boasts the highest concentration. Other areas facing similar challenges include Oxfordshire, Cambridgeshire, Wokingham, Wiltshire, and Central Bedfordshire, all reporting fewer than 15 pharmacies per 100,000 people.
The NPA's research indicates that 87% of council areas in England have experienced at least one pharmacy closure in the past two years. This decline is not isolated to rural areas; nearly all 143 local authorities analyzed have seen a reduction in pharmacies relative to population size, with none reporting an increase.
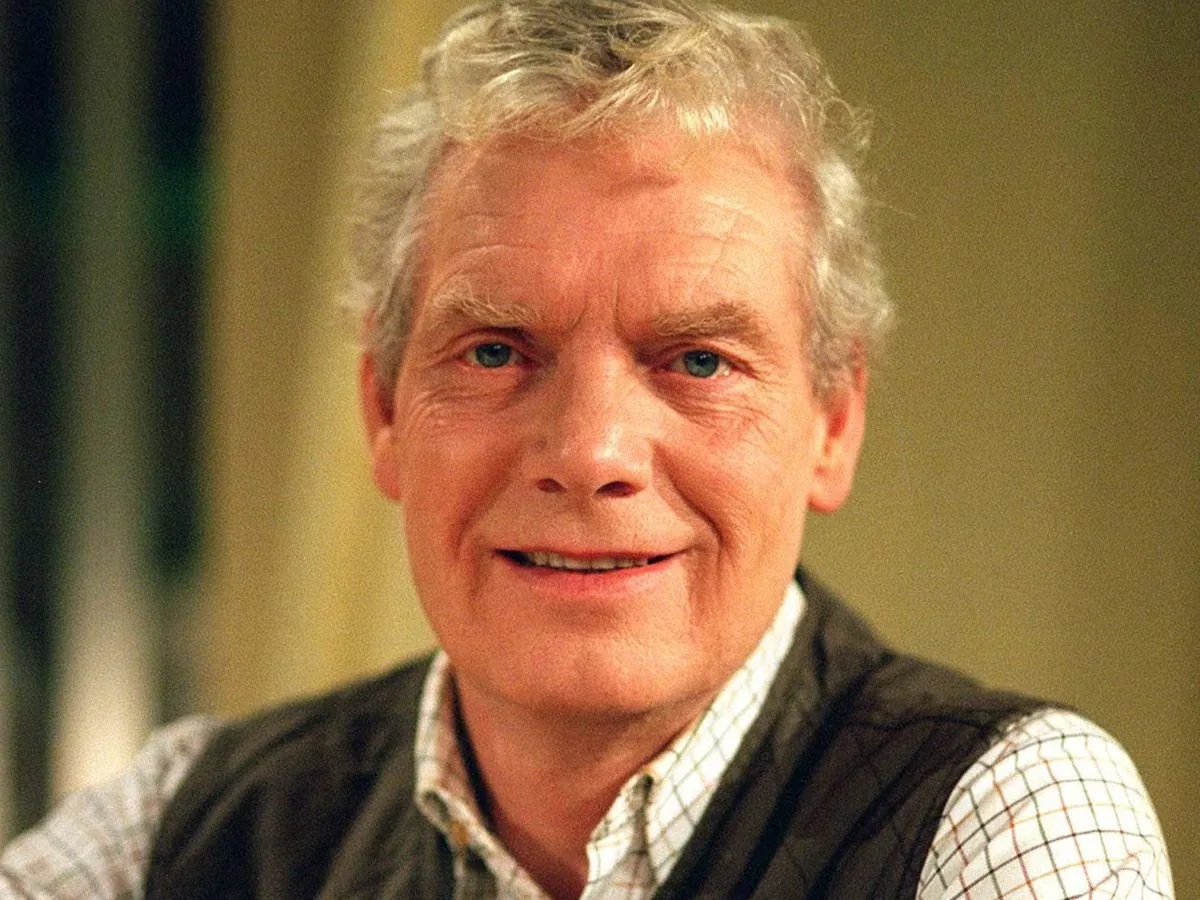
Paul Rees, the NPA's chief executive, expressed deep concern over these findings, stating, "These statistics reveal a growing number of areas at risk of becoming pharmacy deserts, with rural residents facing increasingly longer journeys to access necessary medications."
The root cause of this crisis, according to the NPA, lies in a decade of financial strain on the pharmacy sector. The organization points to what it describes as a 40% real-terms reduction in the pharmacy budget over the past ten years, urging the government to take immediate action to reverse this trend.
David Fothergill, chairman of the Local Government Association's community well-being board, emphasized the multifaceted role of local pharmacies, noting, "People rely on their local pharmacy not just for medicines but as a source of informal health advice and information."
As the situation continues to evolve, there are growing concerns about the impact on health inequalities and the potential strain on other healthcare services. With fewer pharmacies available, there's a risk that more people will turn to already overburdened GP surgeries for services traditionally provided by community pharmacists.
The pharmacy landscape in England has undergone significant changes since the establishment of the first modern pharmacy in London in 1345. Today, with approximately 11,500 community pharmacies serving the nation, the sector faces unprecedented challenges. The growth of online pharmacy services, which have seen a 50% increase since 2020, further complicates the future of traditional brick-and-mortar establishments.
As stakeholders grapple with these issues, the future of rural healthcare accessibility hangs in the balance. The potential emergence of "pharmacy deserts" not only threatens the immediate health needs of rural communities but also challenges the broader goal of equitable healthcare access across England.
"These shocking statistics show how a growing number of areas are at risk of becoming pharmacy deserts, with people in rural towns and villages having to travel longer and longer distances to get hold of the medication they need."