NHS Declines Funding for Groundbreaking Alzheimer's Drug Lecanemab
The NHS won't fund lecanemab, a new Alzheimer's drug that slows cognitive decline, despite regulatory approval. The decision sparks debate on healthcare priorities and access to innovative treatments.

In a recent development, the National Health Service (NHS) has decided not to fund lecanemab, a novel medication for Alzheimer's disease. This decision comes despite the drug receiving approval from the Medicines and Healthcare products Regulatory Agency (MHRA) on August 17, 2024.
Lecanemab, hailed as a significant breakthrough, has demonstrated the ability to slow cognitive decline by 27% in clinical trials. This makes it the first treatment to show evidence of slowing the progression of Alzheimer's disease, a condition first described by German psychiatrist Alois Alzheimer in 1906.
The National Institute for Health and Care Excellence (Nice) cited cost-effectiveness concerns in their draft guidance, stating that the benefits of lecanemab were insufficient to justify its expenses. The treatment, estimated to cost approximately £21,000 per patient, requires additional resources for administration via IV drip and monitoring of side effects.
Hilary Evans-Newton, chief executive at Alzheimer's Research UK, expressed disappointment: "It's clear our health system isn't ready to embrace this new wave of Alzheimer's drugs. It means that, as things stand, people in the early stages of the disease will be denied access to lecanemab through the NHS, and it will only be available to those who can pay privately."
This decision affects an estimated 70,000 adults in England who could have been eligible for the treatment. It's worth noting that Alzheimer's is the most common cause of dementia, accounting for 60-80% of cases, and it's estimated that 50 million people worldwide are living with Alzheimer's or other dementias.

The MHRA's approval comes with certain restrictions. The drug is licensed for patients who do not carry the ApoE4 gene, which is the strongest genetic risk factor for Alzheimer's disease. Patients taking specific blood-thinning medications are also excluded due to increased risk of brain bleeds.
Nice's draft guidance is open for consultation until September 20, 2024. In the meantime, lecanemab will only be available to those who can afford private treatment, which experts believe will be prohibitively expensive for most individuals.
"The costs to obtain the drug privately would be cost prohibitive for all but the most wealthy of individuals."
This situation highlights the ongoing challenges in Alzheimer's treatment and diagnosis. Currently, only 1 in 4 people with Alzheimer's disease have been diagnosed, and in England, one in three people with dementia never receive a formal diagnosis. This underscores the need for improved diagnostic processes within the NHS.
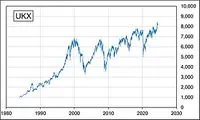
As the global cost of Alzheimer's and dementia is estimated to be $1 trillion annually, the debate over funding innovative treatments like lecanemab is likely to continue. While the drug offers hope by potentially slowing disease progression by 4-6 months, the healthcare system must balance this benefit against its substantial costs.
The decision has sparked calls for further negotiations between Nice, drug manufacturer Eisai, and the NHS to find a solution. As the consultation period progresses, stakeholders will be watching closely to see if a compromise can be reached to make this groundbreaking treatment more accessible to those who need it most.